INHALE Study Scientific Summary
Background
Hospital-acquired and ventilator-associated pneumonias (HAP and VAP) cause a significant excess in morbidity, mortality and costs and affect 1 in 5 ICU patients. The causative microorganism can be bacterial, viral or fungal in nature and conventional diagnosis through bacterial culture can take 2-4 days for a result. Frequently, patients are given a broad-spectrum antibiotic whilst awaiting results from bacterial culture, which often overtreats the pathogen, driving antimicrobial resistance, or undertreats, which may lead to worsened clinical outcomes. INHALE investigated whether the use of molecular diagnostics would improve outcomes in HAP/VAP patients compared to conventional methods.
Objectives:
The main objectives of INHALE were to:
1. Define the accuracy of 3 molecular diagnostic systems, claiming to rapidly identify pathogens and resistance genes in respiratory samples from patients with HAP/VAP, across 4 ICUs.
2. Take the best-performing test from the first objective to conduct an RCT, comparing clinical outcomes and antibiotic use in patients where treatment is guided by the test vs those treated conventionally and refined by microbiological culture.
3. Measure the willingness of clinicians to adopt molecular diagnostic technology and use the results to inform their treatment of patients.
4. To determine if the costs of molecular diagnostics can be justified by the outcomes
WP1 – Clinical Laboratory Evaluation
Methods
Surplus lower respiratory samples from patients with suspected HAP/VAP were tested on the Biofire FilmArray Pneumonia Panel and the Curetis Unyvero Pneumonia panel. Results were compared to routine culture and analysis carried out according to the pre-determined statistical analysis plan using Stata and R.
Results
A total of 652 eligible samples were collected across 15 sites between September 2016 and May 2018. Routine culture provided a result in a median time of 70.2h (IQR 51.1 – 92.1h) and 44.2% of samples tested were positive for likely pathogens. However, there was considerable site-to-site variation observed.
The Unyvero had a positivity rate of 60.4% across 631 eligible samples, whilst the FilmArray had a positivity rate of 74.2% across 632 eligible samples. Both are considerably higher than routine microbiology (p < 0.0001). The range of organisms detected was broadly similar between the PCR and routine microbiology groups.
PCR assay sensitivity was >95% for most of the target bacteria, with NPVs >98%. PPVs and specificity were lower, as the PCR tests detected more organisms per sample and had more positive samples than routine microbiology. Performance parameters were determined by Bayesian Latent Class (BLC) analysis, due to traditional culture representing a poor standard. Routine microbiology was the least sensitive technique and the sensitivity of both PCR tests remained high, whilst specificity and PPV values increased for both PCR tests.
Tests were also evaluated for characteristics such as their speed, size and usability. The FilmArray Pneumonia Panel was chosen during the final decision-making meeting with all stakeholders, for progression into the RCT in WP3.
WP2 - Epidemiology of the Units
Methods
This work was carried out in 4 participating ICUs during WP1 and involved the collection of patient-level and unit-level data.
Participants had an eligible sample included in WP1 and needed to provide consent or assent to participate. Data was collected for up to 21 days after enrolment and was used to determine if the antibiotics prescribed were active and proportionate for the pathogen(s) identified either by PCR or routine culture. Unit-level prescribing and microbiology data was collected from participating ICUs using hospital information systems from October 2016 to December 2017. Data was analysed according to pre-determined plan using Stata and R.
Results
142 participants were recruited (65.5% male; median age 57.9; 24.6% children), 52.1% of which had VAP, whilst the rest had HAP. Of the participants, 86% had received an antibiotic prior to enrolment, over half which were broad-spectrum agents. 51.4% received empirical treatment in accordance with local guidelines, whilst 32.4% received non-guideline empirical therapy and the rest received non-empirical therapy based on a susceptibility result. Regimens commonly used included, piperacillin/tazobactam +/- an aminoglycoside, co-amoxiclav, ceftazidime or ciprofloxacin + teicoplanin. Using the WP2 definition of cure, 62.7% of patients were considered cured of pneumonia at day 21, rising to 74.6% using the WP3 definition, whilst overall mortality at 21 days was 18.3%.
A slightly higher cure rate is shown where treatment was judged to be active, across all three methods. Routine microbiology showed similar cure rates across all stewardship categories, but cure rates were noticeably lower for PCR when an inactive treatment for a positive result was administered, at 48.6% vs 68.9% with active treatment based on FilmArray results (Chi-squared = 4.69, 0=0.03) and 54.1% vs 65.7% based on Unyvero results (Chi-squared = 1.55, p = 0.21).
Adults had a HAP/VAP rate of 22.9 cases/1000 bed days, which was almost double that of children (UCLH ICU). Discrepancies in the positivity rate of samples was observed across hospitals, with UCLH having a ~35% positivity rate, vs ~65% at Cromwell and ~80% at GOSH. Epidemiology of HAP/VAP also varied across sites, with NNUH and UCLH having similar epidemiology to what was expected, whereas Cromwell was significantly different. At Cromwell, epidemiology was dominated by P. aeruginosa and Enterobacterales and a substantial proportion (14%) of A. baumannii. GOSH frequently isolated common community-acquired organisms such as H. influenzae and M. catarrhalis. Prescribing of antibiotics also differed between units.
WP3 – Randomised Controlled Trial
Methods
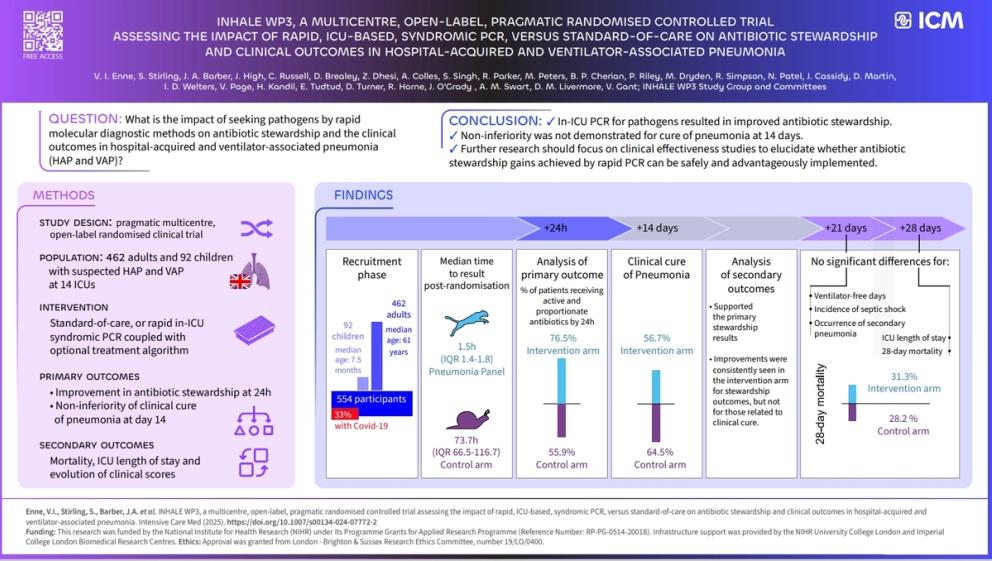
A pragmatic, multicentre, open-label, parallel group, randomised, controlled trial across 14 ICUs, investigating the clinical, safety and cost effectiveness of the FilmArray Pneumonia panel, plus a trial-based prescribing algorithm vs standard care was conducted. Eligible participants were receiving an antibiotic to treat new or worsening HAP/VAP and provided consent or assent to participate.
Intervention arm participants received a Pneumonia Panel test performed at the point of care, alongside the optional treatment algorithm which was designed to promote good antibiotic stewardship. Primary outcomes were equivalence of clinical cure of pneumonia by Day 14 and improvement of antibiotic stewardship at 24h.
Clinical cure rate was assumed at 70% with a non-inferiority margin of 13% but was lowered to 55% following the inclusion of participants with COVID-19. Sample size required was at least 528 participants to achieve 91% power with a significance level of 5% and was inflated to 552 to allow for 5% attrition. Analyses were based on intention-to-treat and followed a pre-defined statistical analysis plan using Stata v17.
Results
554 patients were recruited, 92 of which were children. Primary outcomes were available for 531 participants (median age 61 years for adults; 7.5 months for children) and 33.6% were positive for COVID-19 infection at time of randomisation. Time to result post-randomisation was 1.7h (SD 0.8h) for the Pneumonia Panel vs 110 h (SD 116.2h) for the control arm.
Intention to treat (ITT) analysis for co-primary stewardship outcomes at 24h post-randomisation showed that 76.5% of intervention arm participants were receiving active and proportionate antibiotics by 24h vs 55.9% in the control arm (estimated difference after accounting for site 21%, 95% Confidence interval (CI) 13%-28%, p<0.001). In terms of clinical cure of pneumonia at 14 days, 56.7% of intervention arm participants were considered ‘cured’ vs 64.5% in the control arm (the estimated difference, after accounting for site, was -6% with 95% confidence limits of -15% to 2%). Non-inferiority was not established, as values overlap the non-inferiority margin of 13%.
Secondary outcomes supported primary stewardship results, with improvements in the intervention arm consistently observed. A 28-day mortality of 31.3% was observed in the intervention arm vs 28.2% in the control arm (non-significant difference). No significant differences were observed for duration of ICU stay, ventilator-free days, incidence of septic shock or occurrence of secondary pneumonia across the arms.
WP4 – Behavioural studies
Methods
WP4 was comprised of 4 separate but related behavioural studies utilising mixed methodologies.
Study 1 utilised focus groups and interviews to explore clinicians’ perceptions of antibiotic prescribing in the ICU, using two fictious vignettes of patients with HAP/VAP. Data was analysed by thematic analysis, applying the Necessity Concerns Framework (NCF). Study 2 focused in more detail on clinicians’ beliefs around rapid molecular diagnostic technology ‘in principle’ and its potential in prescribing, using data collected in Study 1. Study 3 explored clinicians’ perceptions of the test in practice using qualitative methods and Study 4 examined whether Pneumonia Panel results influenced individual prescribing decisions for specific patients, and looked to determine clinicians’ beliefs influencing their decision-making, using ecological momentary assessments (EMAs).
Results
When asked about the risks of broad-spectrum antibiotics, few clinicians focused on the potential toxic effects to individual patients, instead, the major concern for broad-spectrum antibiotics was perceived as antimicrobial resistance. However, clinicians were more immediately and profoundly concerned about their patient(s). Use of broad-spectrum antibiotics was an attempt to ‘err on the side of caution’ in order to protect the patient and clinician from the adverse consequences of not prescribing them, which overrode more distal concerns of antimicrobial resistance. Study 3 showed that clinicians had nuanced perceptions of the Pneumonia Panel for treatment of HAP/VAP. Many perceived the value of the test for supporting antibiotic-decision making and antimicrobial stewardship, however, they were concerned about practical application, including false negatives and/or positives. Study 4 highlighted hospital guidelines as one of the most influential factors in antibiotic decision-making. However, 24.9% of decisions were not consistent with local hospital guidelines, demonstrating low confidence in and adherence to them. This was also seen in regards to the WP3 prescribing algorithm, where 67.6% of decisions were not consistent with the algorithm.
WP5 – Health Economic Analysis
Methods
Health economic data was collected for participants of WP2, enabling calculation of costs associated with hospital stays for HAP/VAP. Cost per test for the FilmArray and Unyvero tests were estimated in parallel with WP1.
A review of health economic models from previous studies investigating HAP/VAP costs was carried out. Clinicians were interviewed and a clinical pathway developed, contributing to the development of a bespoke health economic model for INHALE.
Utilising the pre-defined health economic analysis plan, health economic analysis was conducted alongside WP3. Additional costs per additional person on active and proportionate antimicrobial therapy within 24h of clinical diagnosis (“stewardship”) as well as the additional cost per additional clinical cure of pneumonia at 14 days post-randomisation (“cure”) were calculated. Costs were obtained from hospital finance departments and represented hospital income. NHS reference costs were also utilised. Costs were in 2020/21 UK pounds sterling. Early work used to estimate costs of test used in WP1 and 2, were in 2018/19 pounds sterling.
Results
The estimated mean cost of a hospital stay for an adult with HAP/VAP was £42,136, according to work carried out alongside WP2. The Pneumonia Panel test was initially calculated to be £189 but was revised to £198 during WP3. In WP3 the total costs were £40,951 for the control arm vs £32,951 for the intervention arm, amounting to a difference of £8,000(p = 0.472) between the arms. Length of ICU stay was determined to be the largest component of cost. Over a period of 14 days, the intervention arm had a slightly lower associated cost at £19,665 compared to £21,261 in the control arm, a difference of £1,606 (non-significant)(p=0.1835).
The intervention arm had persistently lower costs across all sub-analysis, including separated costs for survivors and those who died. Cost effectiveness for the Pneumonia Panel was demonstrated for antibiotic stewardship but not for clinical cure.
Conclusions
Rapid molecular diagnosis of HAP/VAP was faster and more sensitive than standard care culture. Additional pathogens were detected in PCR, not reported by culture, which could be attributed to a lack of standardisation in interpretation and reporting across hospitals. The Pneumonia Panel was chosen to progress into RCT and placed at the point-of-care in participating ICUs, resulting in increased uptake and recruitment. The Pneumonia Panel improved antimicrobial stewardship by 21% in absolute terms, irrespective of clinicians reservations and was also associated with cost-savings linked to reduced costs for ICU stay.
Equivalence of clinical cure was not demonstrated and clinical outcomes such as SOFA score and mortality didn’t demonstrate any significant differences, but aligned with clinical cure. It is unclear presently if failure to demonstrate clinical cure is due to a small but real effect, another explanation or pure chance. However, to confirm the safety of the intervention, this must be established. To realise the potential of molecular diagnostic technologies in improving AMS, a ‘technology plus’ approach must be taken, to acknowledge the challenges faced by clinicians when applying technological solutions to individual patients’ care.
Future work
Future work should look to determine if the use of the intervention to improve antimicrobial stewardship leads to worse clinical outcomes, the findings of which could have wide-reaching implications and must be further investigated. Currently, work is underway to carry out deeper analysis of existing participants and their data. Inconclusive results may result in a follow-on trial focusing on these clinical outcomes. Future work should also look to support clinicians’ decision making, particularly through the design and development of behavioural materials and interventions. Utilisation of broader diagnostic techniques such as metagenomics may also be of interest, as they would allow a complete overview of the lung microbiome as opposed to focusing on specific pathogens.